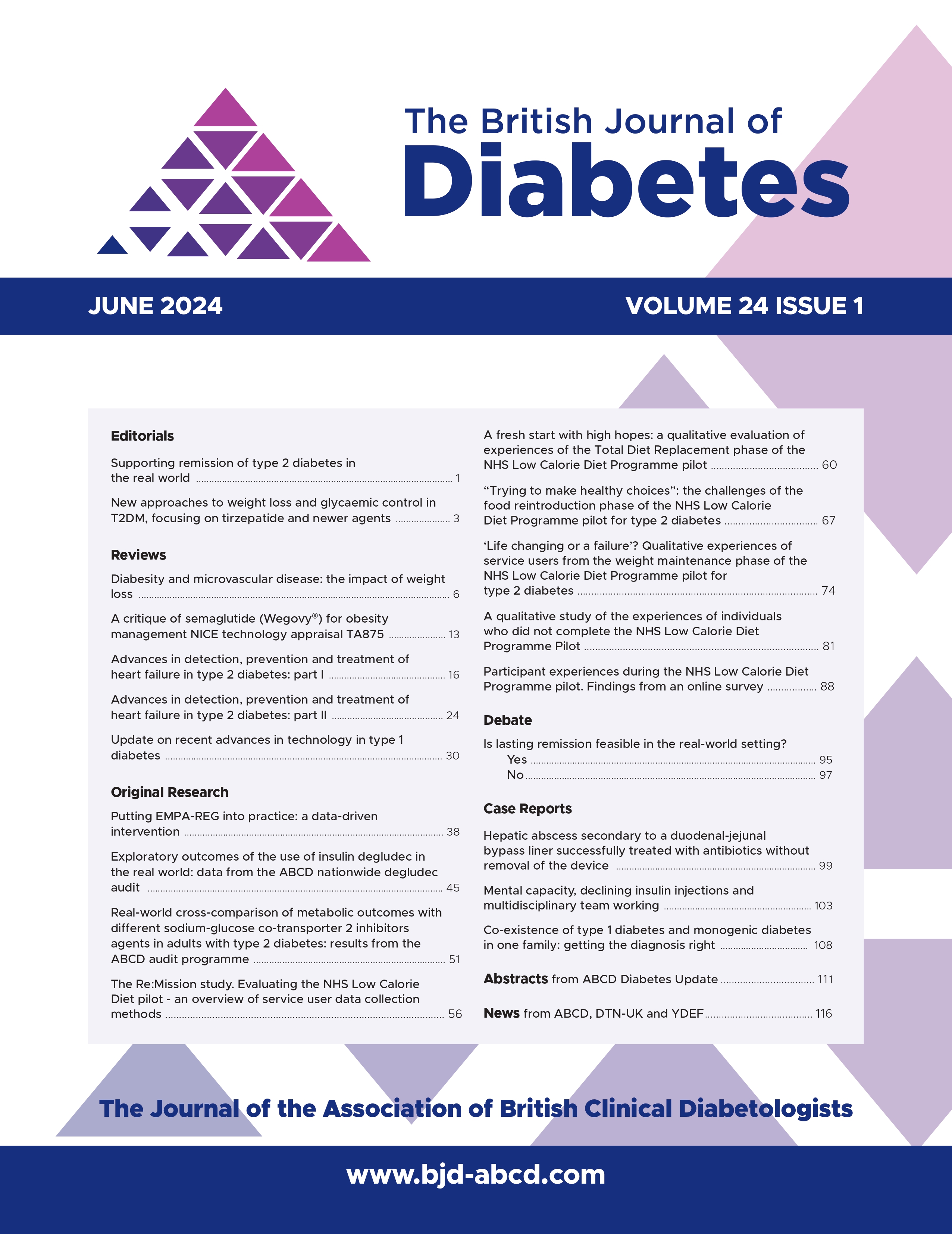
Advances in detection, prevention and treatment of heart failure in type 2 diabetes: part I
DOI:
https://doi.org/10.15277/bjd.2024.441Keywords:
type 2 diabetes, heart failure, heart failure preventionAbstract
Management of heart failure (HF) in diabetes has previously centred on aggressive control of cardiovascular risk factors. The benefits of this approach are modest. In the past decade, however, there have been numerous advances in our understanding of HF prevention, detection and treatment which are particularly relevant to people with type 2 diabetes. This review is the first of two that summarise these advances, with Part I focusing on HF prevention and detection.
References
Rawshani A, Rawshani A, Franzén S, et al. Risk factors, mortality, and cardiovascular outcomes in patients with type 2 NEnglJ Med 2018;379(7):633-44. https://doi.org/10.1056/NEJMoa1800256
Health and Social Care Information Are diabetes services in England and Wales Measuring up? A summary of findings from the National Diabetes Audit 2011–12 for people with diabetes and anyone interested in the quality of diabetes care National Diabetes Audit 2011-12. 2012. hscic.gov.uk/catalogue/PUB12421
(HQIP) THQIP. National Diabetes Audit, 2017-18. Report 2a: Complications and Mortality (complications of diabetes) England and Wales. Healthcare Quality Improvement Partnership. 2017-18. www.hqip.org.uk
(HQIP) THQIP. National Diabetes Audit, 2017-18 Report 2b: Complications and Mortality (characteristics associated with adverse cardiovascular outcomes and diabetic complications) England and 2019. www.hqip.org.uk
Centre HaSCI. National Diabetes Audit 2010-2011 Report 2: Complications and Mortality. 2012. www.digital.nhs.uk
Pop-Busui R, Januzzi JL, Bruemmer D, et al. Heart Failure: an underappreciated complication of A consensus report of the American Diabetes Association. Diabetes Care 2022;45(7):1670-90. https://doi.org/10.2337/dci-0014
Dolgin M, Committee NYHA Criteria Commitee. Nomenclature and criteria for diagnosis of diseases of the heart and great vessels: Little, Brown; Boston, 1994.
McDonagh TA, Metra M, Adamo M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart Eur Heart J 2021;42(36):3599-726. https://doi.org/10.1093/eurheartj/ehab368
Heidenreich PA, Bozkurt B, Aguilar D, et 2022 AHA/ACC/HFSA Guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation 2022; 145(18):e895-e1032. https://doi.org/10.1161/CIR.00000000001063
Hunt SA, Baker DW, Chin MH, et ACC/AHA guidelines for the evaluation and management of chronic heart failure in the adult: executive summary. A report of the American College of Cardiology/American Heart Association task force on practice guidelines (Committee to revise the 1995 guidelines for the evaluation and management of heart failure). Circulation 2001;104(24):2996- 3007. https://doi.org/10.1161/hc4901.102568
Bozkurt B, Coats A, Tsutsui Universal definition and classification of heart failure. J Card Fail 2021;23:352-80. https://doi.org/10.1002/ejhf.2115
Ammar KA, Jacobsen SJ, Mahoney DW, et al. Prevalence and prognostic significance of heart failure Circulation 2007; 115(12):1563-70. https://doi.org/10.1161/CIRCULATIONAHA.106.666818
ACCORDION: long-term follow-up of ACCORD patients. American Heart Association (AHA) 2015 Scientific Sessions; 2015; Orlando,
Castagno D, Baird-Gunning J, Jhund PS, et Intensive glycemic control has no impact on the risk of heart failure in type 2 diabetic patients: evidence from a 37,229 patient meta-analysis. Am Heart J 2011;162(5):938-48.e2. https://doi.org/10.j.ahj.2011.07.030
ACCORD study Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med 2010;362(17):1575-85. https://doi.org/10.1056/NEJMoa1001286
Kamimura D, Cain LR, Mentz RJ, etal. Cigarette smoking and incident heart Circulation 2018;137(24):2572-82. https://doi.org/10.1161/CIRCULATIONAHA.117.031912
Watson M, Dardari Z, Kianoush S, etal. Relation between cigarette smoking and heart failure (from the Multiethnic Study of Atherosclerosis). Am J Cardiol 2019;123(12):1972-7. https://doi.org/1016/j.amjcard.209.03.015
Gopal DM, Kalogeropoulos AP, Georgiopoulou VV, et al. Cigarette smoking exposure and heart failure risk in older adults: The Health, Aging, and Body Composition Study. Am Heart J 2012;164(2):236- https://doi.org/10.1016/j.ahj.2012.05.013
Ahmed AA, Patel K, Nyaku MA, et Risk of heart failure and death after prolonged smoking cessation. Circulation Heart Fail 2015; 8(4):694-701. https://doi.org/10.1161/CIRCHEARTFAILURE.114.001885
Kennedy CD, Van Schalkwyk MCI, McKee M, Pisinger C. The cardiovascular effects of electronic cigarettes: a systematic review of experimental studies. Preventive Medicine 2019;127:105770. https://doi.org/10.1016/j.ypmed.2019.105770
Study links e-cigarette use with higher risk of heart Large study adds to growing body of evidence that vaping may harm the heart [press release]. American College of Cardiology, 2024.
Wei M, Gibbons LW, Kampert JB, Nichaman MZ, Blair Low cardiorespiratory fitness and physical inactivity as predictors of mortality in men with type 2 diabetes. Ann Intern Med 2000; 132(8):605-11. https://doi.org/10.7326/0003-4819-132-8-20004180-00002
Hu FB, Stampfer MJ, Solomon C, et al. Physical activity and risk for cardiovascular events in diabetic Ann Intern Med 2001; 134(2):96-105. https://doi.org/10.7326/0003-4819-134-2-200101160-00009
He J, Ogden LG, Bazzano LA, Vupputuri S, Loria C, Whelton PK. Risk factors for congestive heart failure in US men and women: NHANES I epidemiologic follow-up ArchInternMed 2001;161(7):996- 1002. https://doi.org/10.1001/archinte.161.5.996
Kenchaiah S, Sesso HD, Gaziano Body mass index and vigorous physical activity and the risk of heart failure among men. Circulation 2009;119(1):44-52. https://doi.org/10.1161/CIRCULATIONAHA.108.807289
Hu G, Jousilahti P, Antikainen R, Katzmarzyk PT, Tuomilehto Joint effects of physical activity, body mass index, waist circumference, and waist-to-hip ratio on the risk of heart failure. Circulation 2010; 121(2):237-44. https://doi.org/10.1161/CIRCULATIONAHA.109.887893
Kraigher‐Krainer E, Lyass A, Massaro JM, et Association of physical activity and heart failure with preserved vs. reduced ejection fraction in the elderly: the Framingham Heart Study. Eur J Heart Fail 2013; 15(7):742-6. https://doi.org/10.1093/eurjhf/hft025
Pandey A, Patel M, Gao A, et Changes in mid-life fitness predicts heart failure risk at a later age independent of interval development of cardiac and noncardiac risk factors: The Cooper Center Longitudinal Study. Am Heart J 2015;169(2):290-7.e1. https://doi.org/10.1016/j.ahf.2014.10.017
Khan H, Kunutsor S, Rauramaa R, et Cardiorespiratory fitness and risk of heart failure: a population‐based follow‐up study. Eur J Heart Fail 2014;16(2):180-8. https://doi.org/10.1111/ejhf.37
Florido R, Kwak L, Lazo M, et al. Physical activity and incident heart failure in high‐risk subgroups: the ARIC JournalAmerican Heart Association 2020;9(10):e014885 https://doi.org/10.1161/JAHA.119.014885
Umpierre D, Ribeiro PA, Kramer CK, etal. Physical activity advice only or structured exercise training and association with HbA1c levels in type 2 diabetes: a systematic review and meta-analysis. JAMA 2011; 305(17):1790-9. https://doi.org/10.1001/jama.2011.576
Boule NG, Haddad E, Kenny GP, Wells GA, Sigal RJ. Effects of exercise on glycemic control and body mass in type 2 diabetes mellitus: a meta-analysis of controlled clinical JAMA 2001; 286(10):1218-27. https://doi.org/10.1001/jama.286.10.1218
Colberg SR, Sigal RJ, Yardley JE, et Physical activity/exercise and diabetes: a position statement of the American Diabetes Association. Diabetes Care 2016;39(11):2065-79. https://doi.org/10.2337/dc16-1728
Marx N, Federici M, Schütt K, et al, and ESC Scientific Document 2023 ESC Guidelines for the management of cardiovascular disease in patients with diabetes. Eur Heart J 2023;44:4043-140.. https://doi.org/10.1093/eurheartj/ehad192
Kemps H, Krankel N, Dorr M, et Exercise training for patients with type 2 diabetes and cardiovascular disease: what to pursue and how to do it. A position paper of the European Association of Preventive Cardiology (EAPC). Eur J Prev Cardiol 2019;26:709-27. https://doi.org/10.1177/2047487318820420.
Lee DS, Massaro JM, Wang TJ, etal. Antecedent blood pressure, body mass index, and the risk of incident heart failure in later Hypertension 2007;50(5):869-76. https://doi.org/10.1161/HYPERTENSIONAHA.107.095380
Li W, Katzmarzyk PT, Horswell R, et al. Body mass index and heart failure among patients with type 2 diabetes mellitus. Circulation Heart Failure 2015;8(3):455-63. https://doi.org/10.1161/CIRCHEARTFAILURE.114.001837
Wilding JPH. The importance of weight management in type 2 diabetes Int J Clin Pract 2014;68(6):682-91. https://doi.org/10.1111/ijcp.12384
Wing RR, Lang W, Wadden TA, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 Diabetes Care 2011;34(7):1481-6. https://doi.org/10.2337/dc10-2415
Williamson DF, Thompson TJ, Thun M, Flanders D, Pamuk E, Byers Intentional weight loss and mortality among overweight individuals with diabetes. Diabetes Care 2000;23(10):1499-504. https://doi.org/10.2337/diacare.23.10.1499
Pandey A, Patel KV, Bahnson JL, et al. Association of intensive lifestyle intervention, fitness, and body mass index with risk of heart failure in overweight or obese adults with type 2 diabetes Circulation 2020;141(16):1295-306. https://doi.org/10.1161/CIRCULATIONAHA.119.044865
Look ARG, Wing RR, Bolin P, et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med 2013; 369(2):145-54. https://doi.org/10.1056/NEJMoa1212914
Look ARG, Gregg EW, Jakicic JM, etal. Association of the magnitude of weight loss and changes in physical fitness with long-term cardiovascular disease outcomes in overweight or obese people with type 2 diabetes: a post-hoc analysis of the Look AHEAD randomised clinical trial. Lancet Diabetes Endocrinol 2016;4(11):913-21. https://doi.org/10.1016/S2213-8586(16)30162-0
Patel KV, Bahnson JL, Gaussoin SA, et Association of baseline and longitudinal changes in body composition measures with risk of heart failure and myocardial infarction in type 2 diabetes: findings from the Look AHEAD Trial. Circulation 2020;142(25):2420-30. https://doi.org/10.1161/CIRCULATIONAHA.120.050941
Diallo A, Villard O, Carlos-Bolumbu M, Renard E, Galtier Effects of hypoglycaemic agents on reducing surrogate metabolic parameters for the prevention of cardiovascular events and death in patients with type 2 diabetes: a systematic review and meta-analysis. Diabetes Obes Metab 2023;26:495-502. https://doi.org/10.1111/dom.15335
Jastreboff AM, Aronne LJ, Ahmad NN, etal. Tirzepatide once weekly for the treatment of obesity. N Engl J Med 2022;387(3):205-16. https://doi.org/10.1056/NEJMoa2206038
Garvey WT, Frias JP, Jastreboff AM, et Tirzepatide once weekly for the treatment of obesity in people with type 2 diabetes (SURMOUNT-2): a double-blind, randomised, multicentre, placebo- controlled, phase 3 trial. Lancet 2023;402(10402):613-26. https://doi.org/10.1016/S0140-6736(23)01200-X
Wilding JPH, Batterham RL, Calanna S, et al. Once-weekly semaglutide in adults with overweight or N Engl J Med 2021; 384(11):989. https://doi.org/10.1056/NEJMoa2032183
Pi-Sunyer X, Astrup A, Fujioka K, et A randomized, controlled trial of 3.0 mg of liraglutide in weight management. N Engl J Med 2015; 373(1):11-22. https://doi.org/10.1056/NEJMoa1411892
Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and cardiovascular outcomes in type 2 N Engl J Med 2016; 375(4):311-22. https://doi.org/10.1056/NEJMoa1603827
Marso SP, Bain SC, Consoli A, et Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med 2016; 375(19):1834-44. https://doi.org/10.1056/NEJMoa1607141
Lincoff AM, Brown-Frandsen K, Colhoun HM, et al. Semaglutide and cardiovascular outcomes in obesity without N Engl J Med 2023;389:2221-32. https://doi.org/10.1056/NEJMoa2307563
Lee MMY, Sattar N, McMurray JJV, Packard CJ. Statins in the prevention and treatment of heart failure: a review of the Current Atherosclerosis Reports 2019;21(10):41. https://doi.org/10.1007/s11883-019-0800-z
Lakoumentas JA, Dimitroula TG, Aggeli KI, Harbis Cholesterol levels and the benefit of statins in heart failure. Hellenic J Cardiol 2005;46(3):226-31.
Colhoun HM, Betteridge DJ, Durrington PN, et al. Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): multicentre randomised placebo-controlled Lancet 2004;364(9435):685-96. https://doi.org/10.1016/S0140-6736(04)16895-5
SSSS Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet 1994;344:1383-9. https://doi.org/1016/S0140-6736(94)90566-5
Low Wang CC, Hess CN, Hiatt WR, Goldfine Clinical update: cardiovascular disease in diabetes mellitus. Circulation 2016;133 (24):2459-502. https://doi.org/10.1161/CIRCULATIONAHA.116.022194
Filippatos TD, Mikhailidis Statins and heart failure. Angiology 2008;59(2 Suppl):58s-61s. https://doi.org/10.1177/0003319708319643
Bielecka-Dabrowa A, Bytyçi I, Von Haehling S, et al. Association of statin use and clinical outcomes in heart failure patients: a systematic review and meta-analysis. Lipids in Health and Disease 2019;18(1):188. https://doi.org/10.1186/s12944-019-1135-z
Schwartz GG, Steg PG, Szarek M, et al. Alirocumab and cardiovascular outcomes after acute coronary N Engl J Med 2018;379(22):2097-107. https://doi.org/10.1056/NEJMoa1801174
JBS3 Summary of national guidance for lipid management for primary and secondary prevention of CVD. In: Collaborative NHSAA, editor. 2024.
Niessner A, Drexel PCSK9 inhibition in patients with heart failure: neutral or harmful intervention? Eur Heart J 2022;43(16):1566-8. https://doi.org/10.1093/eurheartj/ehab913
Da Dalt L, Castiglioni L, Baragetti A, etal. PCSK9 deficiency rewires heart metabolism and drives heart failure with preserved ejection Eur Heart J 2021;42(32):3078-90. https://doi.org/10.1093/eurheartj/ehab431
Cegla National Institute for Health and Care Excellence guidelines for lipid management. Heart 2023;109(9):661-7. https://doi.org/10.1136/heartjnl-2022-321414
Echouffo-Tcheugui JB, Ndumele CE, Zhang S, et Diabetes and progression of heart failure: the Atherosclerosis Risk In Communities (ARIC) Study. J Am Coll Cardiol 2022;79(23):2285-93. https://doi.org/10.1016/j.jacc.2022.03.378
Lind M, Olsson M, Rosengren A, Svensson AM, Bounias I, Gudbjörnsdottir The relationship between glycaemic control and heart failure in 83,021 patients with type 2 diabetes. Diabetologia 2012;55(11):2946-53. https://doi.org/10.1007/s00125-012-2681-3
ADVANCE Collaborative Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) Group. Lancet 1998;352(9131):854-65.
Group AC, Patel A, MacMahon S, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 N Engl J Med 2008;358(24):2560-72. https://doi.org/10.1056/NEJMoa0802987
Action to Control Cardiovascular Risk in Diabetes Study Group; Gerstein HC, Miller ME, Byington RP, et al. Effects of intensive glucose lowering in type 2 N Engl J Med 2008;358(24):2545-59. https://doi.org/10.1056/NEJMoa0802743
Duckworth W, Abraira C, Moritz T, et Glucose control and vascular complications in veterans with type 2 diabetes. NEnglJMed 2009; 360(2):129-39. https://doi.org/10.1056/NEJMoa0808431
Control Group; Turnbull FM, Abraira C, Anderson RJ, et Intensive glucose control and macrovascular outcomes in type 2 diabetes. Diabetologia 2009;52(11):2288-98. https://doi.org/10.1007/s00125-009-1470-0
ElSayed NA, Aleppo G, Aroda VR, et al. Cardiovascular disease and risk management: standards of care in diabetes-2023. Diabetes Care 2023;46(Suppl 1):S158-S90. https://doi.org/10.2337/dc23-S010
Cosentino F, Grant PJ, Aboyans V, et 2019 ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J 2020;41(2):255-323. https://doi.org/10.1093/eurheartj/ehz486
Type 2 diabetes in adults: management. 2015. PMID:26741015
Joseph JJ, Deedwania P, Acharya T, et al. Comprehensive management of cardiovascular risk factors for adults with type 2 diabetes: a scientific statement from the American Heart Association. Circulation 2022;145(9): e722-e759. https://doi.org/10.1161/CIR00000000001040
Zinman B, Wanner C, Lachin JM, etal. Empagliflozin, cardiovascular outcomes, and mortality in type 2 N Engl J Med 2015;373(22):2117-28. https://doi.org/10.1056/NEJMoa1504720
Wiviott SD, Raz I, Bonaca MP, et Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med 2019;380:347-57. https://doi.org/10.1056/NEJMoa1812389
Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and cardiovascular and renal events in type 2 N Engl J Med 2017;377(7):644-57. https://doi.org/10.1056/NEJMoa1611925
McGuire DK, Shih WJ, Cosentino F, et al. Association of SGLT2 inhibitors with cardiovascular and kidney outcomes in patients with type 2 diabetes: a meta-analysis. JAMA Cardiol 2021;6(2):148-58. https://doi.org/10.1001/jamacardio.2020.4511
Holman RR, Bethel MA, Mentz RJ, et al. Effects of once-weekly exenatide on cardiovascular outcomes in type 2 N Engl J Med 2017;377(13):1228-39. https://doi.org/10.1056/NEJMoa1612917
Hernandez AF, Green JB, Janmohamed S, et al. Albiglutide and cardiovascular outcomes in patients with type 2 diabetes and cardiovascular disease (Harmony Outcomes): a double-blind, randomised placebo-controlled trial. Lancet 2018;392:1519-29. https://doi.org/10.1016/S0140-6736(18)32261-X
Husain M, Birkenfeld AL, Donsmark M, et Oral semaglutide and cardiovascular outcomes in patients with type 2 diabetes. NEnglJ Med 2019;381:841-51. https://doi.org/10.1056/NEJMoa1901118
Ferreira JP, Saraiva F, Sharma A, et al. Glucagon-like peptide 1 receptor agonists in patients with type 2 diabetes with and without chronic heart failure: a meta-analysis of randomized placebo- controlled outcome trials. Diabetes Obes Metab 2023;25(6): 1495-502. https://doi.org/10.1111/dom.14997
Bayés-Genís A, Díez Transition to heart failure in hypertension: going to the heart of the matter. EurHeartJ 2022;43(35):3332-4. https://doi.org/10.1093/eurheartj/ehab651
Goyal A, Norton CR, Thomas TN, et al. Predictors of incident heart failure in a large insured population: a one million person-year follow- up study. Circ Heart Fail 2010;3(6):698-705. https://doi.org/10.1161/110.938175
Ahmad FS, Ning H, Rich JD, Yancy CW, Lloyd-Jones DM, Wilkins Hypertension, obesity, diabetes, and heart failure-free survival: the Cardiovascular Disease Lifetime Risk Pooling Project. JACC Heart Fail 2016;4(12):911-19. https://doi.org/10.1016/j.jchf.2016.08.001
Folsom AR, Yamagishi K, Hozawa A, Chambless Absolute and attributable risks of heart failure incidence in relation to optimal risk factors. Circulation Heart Failure 2009;2(1):11-17. https://doi.org/10.1161/CIRCHEARTFAILURE.108.794933
The SPRINT Research A randomized trial of intensive versus standard blood-pressure control. N EngJ Med 2015;373(22):2103-16. https://doi.org/10.1056/NEJMoa1511939
Hypertension in adults: diagnosis and management. 2019. NG136
Weinstock RS, Trief PM, Burke B, etal. Antihypertensive and lipid- lowering medication adherence in young adults with youth-onset type 2 diabetes. JAMA Network Open 2023;6(10):e2336964. https://doi.org/10.1001/jamanetworkopen.2023.36964
Gupta P, Patel P, Štrauch B, et al. Risk factors for nonadherence to antihypertensive Hypertension 2017;69(6):1113-20. https://doi.org/10.1161/HYPERTENSIONAHA.116.08729
Gupta P, Patel P, Horne R, Buchanan H, Williams B, Tomaszewski How to screen for non-adherence to antihypertensive therapy. Current Hypertension Reports 2016;18(12):89. https://doi.org/10.1007/s11906-016-0697-7
Boonman-de Winter LJ, Rutten FH, Cramer MJ, et High prevalence of previously unknown heart failure and left ventricular dysfunction in patients with type 2 diabetes. Diabetologia 2012;55(8):2154-62. https://doi.org/10.1007/s00125-012-2579-0
Echouffo-Tcheugui JB, Erqou S, Butler J, Yancy CW, Fonarow Assessing the risk of progression from asymptomatic left ventricular dysfunction to overt heart failure: a systematic overview and meta- analysis. JACC Heart Fail 2016;4(4):237-48. https://doi.org/10.1016/j.jchf.2015.09.015
Young KA, Scott CG, Rodeheffer RJ, Chen HH. Progression of preclinical heart failure: a description of stage A and B heart failure in a community population. Circ Cardiovasc Qual Outcomes 2021; 14(5):e007216. https://doi.org/10.1161/CIRCOUTCOMES.120.007216
Gulsin GS, Athithan L, McCann GP. Diabetic cardiomyopathy: prevalence, determinants and potential treatments. Ther Adv Endocrinol Metab 2019;10:2042018819834869. https://doi.org/10.1177/204201881983489
Dattani A, Joshi S, Yeo JL, et Impaired myocardial calcium uptake in patients with diabetes mellitus: a manganese-enhanced cardiac magnetic resonance study. JACC Cardiovasc Imaging 2023; 16(12):1623-5. https://doi.org/10.1016/j.jcmg.202.05.009
SCORE2-Diabetes Working Group and the ESCCRC. SCORE2- Diabetes: 10-year cardiovascular risk estimation in type 2 diabetes in Eur Heart J 2023;44(28):2544-56. https://doi.org/10.1097/eurheartj/ehad260
Pandey A, Khan MS, Patel KV, Bhatt DL, Verma S. Predicting and preventing heart failure in type 2 diabetes. Lancet Diabetes Endocrinol 2023;11(8):607-24. https://doi.org/10.1016/S2213-8587(23)00128-6
Azimova K, San Juan Z, Mukherjee D. Cardiovascular safety profile of currently available diabetic OchsnerJ 2014;14(4):616-32. PMID:25598727
Jensen MT, Fung K, Aung N, etal. Changes in cardiac morphology and function in individuals with diabetes mellitus: the UK Biobank cardiovascular magnetic resonance substudy. Circ Cardiovasc Imaging 2019;12(9):e009476. https://doi.org/10.1161/119.009476
Robinson S, Rana B, Oxborough D, et A practical guideline for performing a comprehensive transthoracic echocardiogram in adults: the British Society of Echocardiography minimum dataset. Echo Res Pract 2020;7(4):G59-G93. https://doi.org/10.1530/ERP-20-0026
Mitter SS, Shah SJ, Thomas A test in context: E/A and E/e' to assess diastolic dysfunction and LV filling pressure. J Am Coll Cardiol 2017;69(11):1451-64. https://doi.org/10.1016/j.jacc.2016.12.037
Verbrugge FH, Omote K, Reddy YNV, Sorimachi H, Obokata M, Borlaug Heart failure with preserved ejection fraction in patients with normal natriuretic peptide levels is associated with increased morbidity and mortality. Eur Heart J 2022;43(20):1941-51. https://doi.org/10.1093/eurheartj/ehab911
Ohkuma T, Jun M, Woodward M, et al. Cardiac stress and inflammatory markers as predictors of heart failure in patients with type 2 diabetes: the ADVANCE Diabetes Care 2017;40(9):1203-9. https://doi.org/10.2337/dc17-0509
Bojer AS, Sørensen MH, Gæde P, Madsen PL. Myocardial extracellular volume expansion in type 2 diabetes is associated with ischemic heart disease, autonomic neuropathy, and active Diabetes Care 2022;45(12):3032-9. https://doi.org/10.2337/dc22-0942
Gulsin GS, Swarbrick DJ, Athithan L, etal. Effects of low-energy diet or exercise on cardiovascular function in working-age adults with type 2 diabetes: a prospective, randomized, open-label, blinded end point trial. Diabetes Care 2020;43(6):1300-10. https://doi.org/2337/dc20-0129
Liakopoulos V, Franzén S, Svensson AM, et al. Renal and cardiovascular outcomes after weight loss from gastric bypass surgery in type 2 diabetes: cardiorenal risk reductions exceed atherosclerotic benefits. Diabetes Care 2020;43(6):1276-84. https://doi.org/10.2337/dc19-1703
Skali H, Shah A, Gupta DK, et al. Cardiac structure and function across the glycemic spectrum in elderly men and women free of prevalent heart disease: the Atherosclerosis Risk In the Community Circ Heart Fail 2015;8(3):448-54. https://doi.org/10.1161/CIRCHEARTFAILURE.114.001990.
Published
Issue
Section
License
Copyright (c) 2024 British Journal of Diabetes

This work is licensed under a Creative Commons Attribution 4.0 International License.
Manuscripts published in the June 2024 edition and after in the BJD have been published in open access under a Creative Commons Attribution 4.0 International License and available at https://www.bjd-abcd.com. Prior year articles are available free of charge via our website.